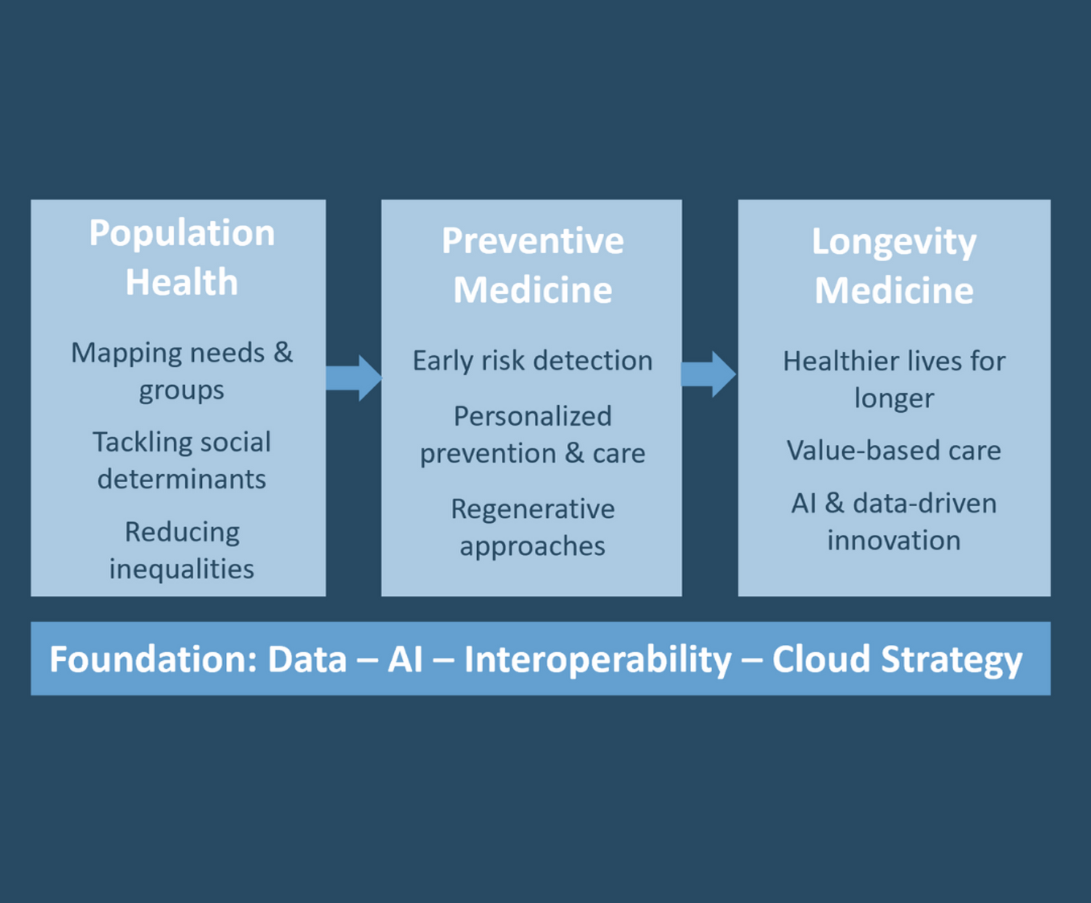
Population Health
Population health looks at entire groups, whether defined by geography, demographics, or health status, to identify individuals at risk or those who have been left out of screenings and preventive programs.
These initiatives also address the social determinants of health, such as income, education, environment, and access to care. By uncovering inequities between groups, they create opportunities to reduce disparities across the population.
From an economic perspective, population health programs help control healthcare spending by preventing avoidable hospitalizations and improving the management of chronic diseases.
In short, population health keeps people healthier for longer by combining prevention, data-driven risk detection, coordinated care, and attention to both medical and social needs.
Preventive and Longevity Medicine
Preventive and longevity medicine is emerging as one of the most significant medical revolutions of the coming decades. It provides a strategic response to the mounting challenges of public health.
By integrating genomics, biotechnology, and regenerative medicine, this approach enables ultra-personalized care: identifying risks early, tailoring treatments, and regenerating tissues damaged by aging.
Modern personalized preventive medicine, closely aligned with precision medicine, seeks to adapt prevention, diagnosis, and treatment to each person’s unique biology. It relies on genetics, biomarkers, environment, and lifestyle data to guide decisions.
Scaling Preventive and Longevity Medicine
The next step is deploying preventive and longevity medicine on a large scale. To achieve this, two pillars are essential: population health programs and value-based care.
Population health will map medical needs across different territories and groups, embedding social determinants into a holistic strategy.
Value-based care will align healthcare providers with models that reward quality, outcomes, and cost control rather than the volume of services delivered.
The data already used in today’s population health programs will, with greater computing power and over longer time horizons, serve as the basis for preventive and longevity medicine. This will require robust interoperability platforms, deployed at scale, with strong security and compliance with European regulations.
Technology as the Foundation
Digital technologies are accelerating this transformation, making innovation accessible to more people and paving the way for a modern, integrated, and efficient healthcare system. This system is built around prevention, early detection, and sustainable, personalized care throughout the patient journey.
At the heart of this transformation lies digital health data. It is both the content and the container of modern healthcare: the backbone of hospitals, clinics, and community practices; the digital twin of the patient; and the daily tool of healthcare professionals. Health data drives scientific progress and, with the help of AI, opens vast opportunities for research, innovation, diagnosis, treatment, and cost optimization.
The European Challenge
In Europe, and especially in France, we have fallen behind in the race for big data and are not leading in smart data or in the application of AI to healthcare. Closing this gap with the world’s most advanced nations demands a pragmatic approach, particularly regarding cloud strategy.
We must balance legitimate concerns for security and sovereignty with the need for innovation and speed to market. Not all healthcare data must be stored in sovereign clouds, nor must all services be confined there. A more effective solution could be a multi-cloud strategy, relying heavily on open-source solutions while integrating the most powerful interoperability platforms available today.
One critical gap Europe must bridge, especially in preventive and longevity medicine, is the use of large language models (LLMs) trained primarily on non-European healthcare datasets. To ensure relevance, trust, and sovereignty, it is urgent to develop the capability to train these models on territory-based health data. This will likely require the same multi-cloud strategy, underpinned by powerful interoperability platforms, to enable secure, large-scale, and regulation-compliant training environments.


Hicham Temsamani
Hicham Temsamani is a biomedical engineer with extensive international experience in the health sector. After a career at the French National Space Agency (CNES), and then at Panasonic, Cisco, Cardinal Health, AWS and Google Cloud, he founded H.B.T Group France – his strategic consulting firm specialized in digital transformation for healthcare organizations. Passionate about innovation and prevention, he also hosts scientific conferences focused on preventive medicine and longevity.